THE IMPACT OF MY UK EXPERIENCES
Michael shares his experiences of BSH and haematology practice in the UK:
My visit to the UK was one experience out of the ordinary. It was life changing! I must specially commend my UK friends for their unwavering commitment and tender support that enabled the success of this visit. The BSH event was overwhelmingly exciting and I was so touched by the exquisite organization, quality and hospitality of the conference, kudos to the organizers! Queen’s Hospital was such a wonderful place to be, so cool, so soothing and so radiant, never a dull moment. I got deeply impressed by the humility, kindness and warmth of the staff especially the doctors and nurses. Their display of teamwork, motivation and professionalism which struck a note of harmonious relationship was simply amazing!
1. MEDICAL PRACTICE
Renewed determination: My short clinical experience and few conferences have reinforced my resolve to pursue excellence in my career and life in general against the odds. I realized that excellence constitutes doing ordinary things in an extraordinary way. Dedication to patient care was rekindled and a renewed commitment for breakthroughs activated.
Working smart: The very moment I arrived UK, I perceived technology at work. I couldn’t help noticing the immense gap between the NHS and the Nigerian version. The former being far more efficient and smarter by deploying ICT and other scientific innovations. This stark discovery has spurred me to upgrade ICT capabilities and advocate for greater uptake of ICT in our hospitals to improve service delivery, job satisfaction and overall performance.
Time management: In UK, time discipline was just a way of life. The impact on productivity can never be overemphasized. I really struggled to keep up. Realizing once more the critical importance of time-consciousness and prioritization of tasks has kept me working on my time habits thus helping me make headway while avoiding embarrassments.
Informed consent/counseling: Often taken for granted in our setting but thanks to the exposure in Queen’s, I was reaffirmed of the importance of carrying along the patient and caregivers/families in the decision making and treatment process. Effective communication and consent can save a whole lot of trouble and returns a better outcome.
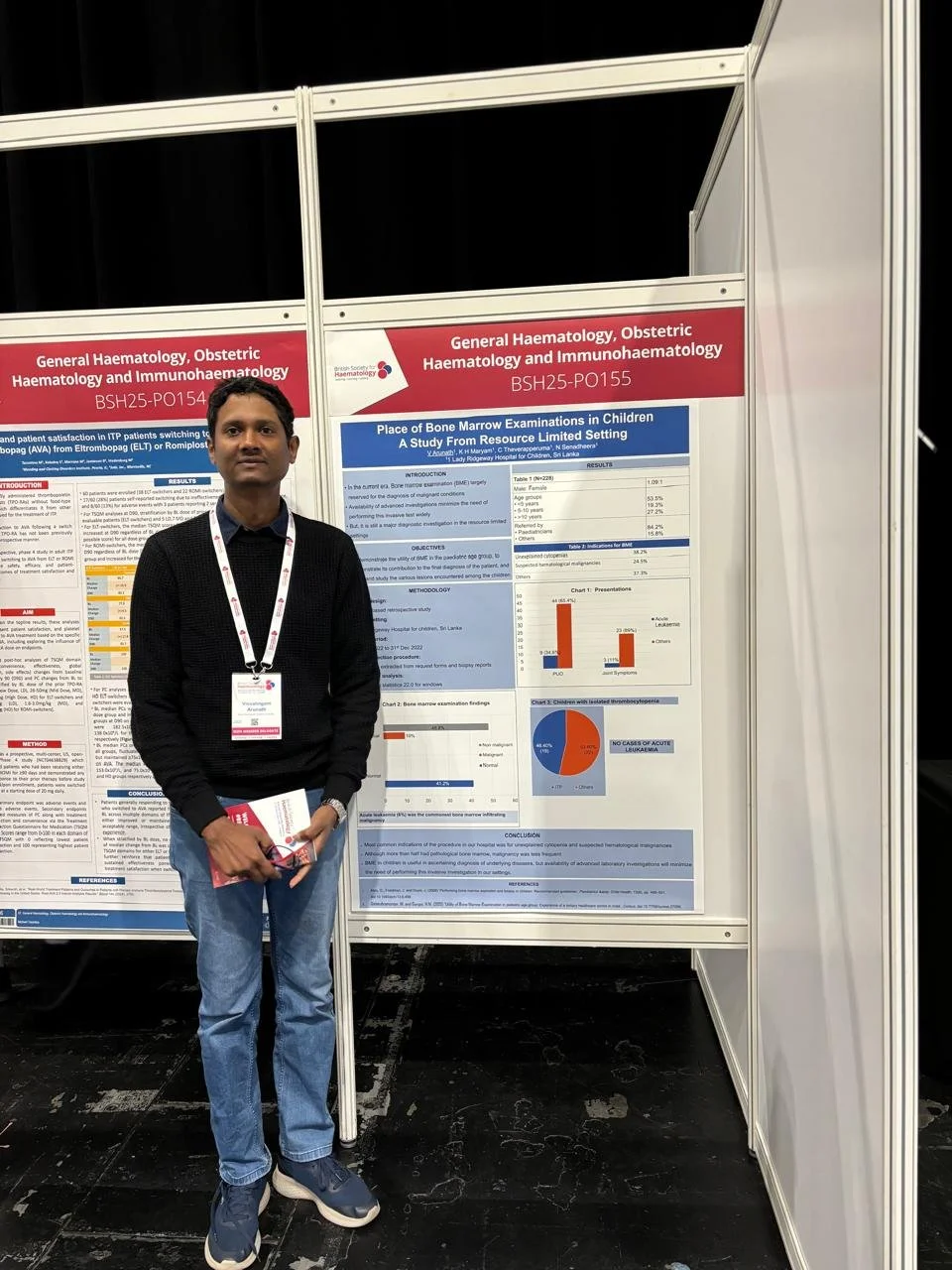
Skill acquisition: My skills with several haematological procedures like BMA and biopsy, slide preparation, microscopy were sharpened. I witnessed a live apheresis session for red cell exchange in an SCD patient which has deepened my insight in applications of apheresis.
2. HAEMRYNE NETWORK
Inspiration: My zeal was reinforced for our nascent network after experiencing the warm reception and massive hospitality of the HaemSTAR. Their productive cooperation and synergy was a big eye opener for exploiting potentials of networking and collaboration. I have a vision. I see lots of potentials in HaemRYNE!
Delegation of duties: I observed how assignment of specific roles and division of labour translated into efficiency and productivity. The HaemSTAR is structured thus. Back home I have resolved to introduce this sharing of responsibilities to our network, in our hospitals too and even in other aspects of live. We call it divide and conquer!
Record keeping: Data retrieval was the success key for most of the HaemSTAR’s audit projects thus underscoring the utmost importance of record keeping which unfortunately is still crude in my clime. I have borrowed a leaf from the UK’s model and hope to incorporate good data collection, processing and information storage in the HaemRYNE and our respective hospital settings.
Many thanks to BSH and HaemSTAR to whom I am highly indebted.